
As Americans age, their desire to stay in their homes remains steadfast. According to the AARP, 77% of adults aged 50 and older want to remain in their homes for the long term — a number that has remained unchanged for more than 10 years now.
But unexpected medical events and declines in health can make it challenging to remain safe and well cared for at home. For example, most homes are not designed to support aging in place. In fact, 34% of older adults say they may need to make physical changes to their house, such as modifying a bathroom or installing ramps in their homes to live there independently for as long as possible.
And, as people age, they increasingly need support with activities of daily living like shopping, bathing, and cleaning. While there are a number of organizations that can deliver these services, access is difficult due to pre-authorization requirements and staff turnover with many providers.
MA Plans Lean Into In-Home Services
As care continues to move to the home, the healthcare system will have to find ways to support people who are aging in place. There is a clear opportunity for Medicare Advantage (MA) plans to provide home-centered services that are high quality and easy to access – and data shows that many plans are leaning in.
MA plans have seen a 35% upswing in supplemental benefits nationwide – most notably for in-home services. Regulatory changes now enable MA plans to offer members expanded non-medical supplemental benefits, including those that address health-related social needs and social determinants of health.
In addition, enrollment in MA Special Needs Plans (SNP) has grown by more than twofold from 2020 to 2022. SNPs provide benefits and services to people with specific diseases, certain health care needs, or who also have Medicaid. For example, there are SNPs for individuals who are dually eligible (D-SNPs, i.e., for members eligible for Medicare and Medicaid), those with chronic conditions (C-SNPs), and patients in institutional settings or who require institutional care (I-SNPs). These plans are increasingly looking at ways to support their membership’s desire to age-in-place, and tailor their benefits, provider choices, and list of covered drugs to best meet the needs of the groups they serve.
Creating an Aging-in-Place Strategy: 5 Steps
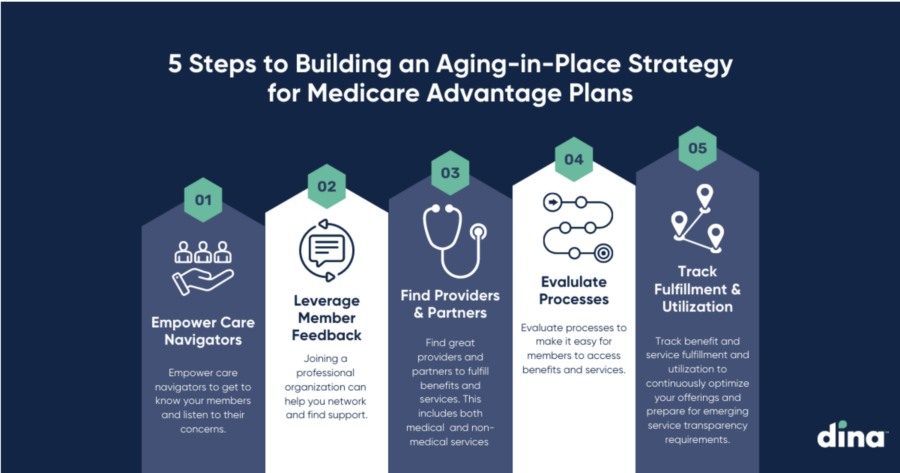
The upward trend around the delivery of in-home medical and non-medical services is expected to continue and MA plans should prepare to manage this shift in healthcare delivery. This often starts with a cohesive aging-in-place strategy to drive growth. Here are five steps to get started:
- Empower care navigators to get to know your members and listen to their concerns.
- Use member feedback to inform plan design and add services that meet their needs.
- Find great providers and partners to fulfill benefits and services. This includes both medical services like home health and hospice, and non-medical services like IHSS providers, home modification, meals and nutrition, transport, and respite care.
- Evaluate processes to make it easy for members to access benefits and services.
- Track benefit and service fulfillment and utilization to continuously optimize your offerings and prepare for emerging service transparency requirements.
People have choices when it comes to what kind of healthcare they want, how and where they access it, and which insurance plan is the best fit. In response, the challenge for payers is to unlock new benefits to meet members where they are on their healthcare journey to help them live their very best life.




