Many hospitals and health systems are trying to determine how to implement successful care-at-home initiatives. While these at-home care models aren’t new, interest has skyrocketed due to the impact of the COVID-19 pandemic. And though it’s not for every patient or every condition, many opportunities exist to transfer certain care to the lowest-cost, most-convenient option: the home.
During a recent webinar hosted by Becker’s Hospital Review, industry leaders from Philadelphia-based Jefferson Health and Chicago-based Dina discussed the expansion of home-based care, which virtual services Medicare reimburses, and keys to building a successful Hospital-at-Home program.
Four takeaways:
- The rise of home-based care. Several market forces are shifting care to lower-cost environments, with patients’ homes arguably the lowest-cost, most convenient setting. President Joe Biden’s American Jobs Plan features a $400 billion investment to expand access to Medicaid home and community-based services for older adults and people with disabilities, which would enhance programs that allow patients to receive care at home.
“It’s become more important for health systems and provider groups to really develop competent care delivery models that can actually deliver on lower cost, higher quality of care,” said Dr. Kate Behan, senior vice president and chief population health officer at Jefferson Health.
- More virtual services are being reimbursed. Telehealth is one component of virtual care that has significantly expanded over the past year. Now, there are more than 135 services that can be covered via telehealth, including emergency department visits, inpatient nursing facility visits, remote patient monitoring and discharge day management services, according to Dina CEO Ashish V. Shah. “These services can all be delivered and then reimbursed via telehealth,” he said.
Remote patient monitoring, for example, has expanded CPT codes to reimburse providers for time spent and equipment used to deliver care, including training and onboarding services
- Hospital-at-Home expands. The Acute Hospital Care at Home program, an expansion of CMS’ Hospital Without Walls initiative launched in March 2020, is designed to increase hospitals’ capacity to provide care outside the inpatient setting and within a patient’s home. There are currently 56 systems and 129 hospitals enrolled in the program, which “creates an opportunity for hospitals, health systems or other providers” to receive payment for at-home treatment that’s equal to what they would receive if the patient was treated in a hospital.
Successful outcomes require hospitals to reimagine the post-acute experience.
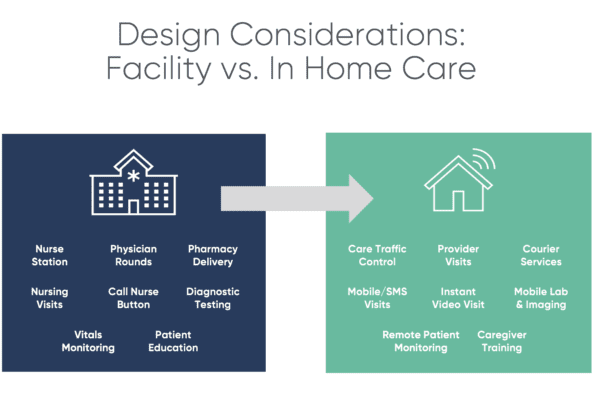
There are up to 60 conditions, including asthma, pneumonia and congestive heart failure, that can be treated at home through the initiative. Successful outcomes require hospitals to reimagine the post-acute experience, Shah said. This means replicating the hospital room with a marketplace of home-based services including telehealth, remote patient monitoring, courier services, home modifications, pharmacy, home infusion, non-medical home care and mobile imaging/radiology.
- Evaluating at-home models. There is no one-size-fits-all solution for healthcare organizations that want to establish a Hospital-at-Home model. Key pillars to ensuring the success of these programs include: establishing a geographical fit; aligning with innovative payers, hospital finance and contracting teams; and researching targeted patient populations for launch, according to Kristen Vogl, Jefferson Health’s enterprise vice president of post-acute care and musculoskeletal services.
It’s also critical to install executive champions capable of developing and executing the vision. “You want to maximize your expertise and your resources to make this work,” she said.
Read more here about how leading health systems like Jefferson Health prepare for a shift to home-based care. And, you can watch the webinar here.