
Opportunity to jump in
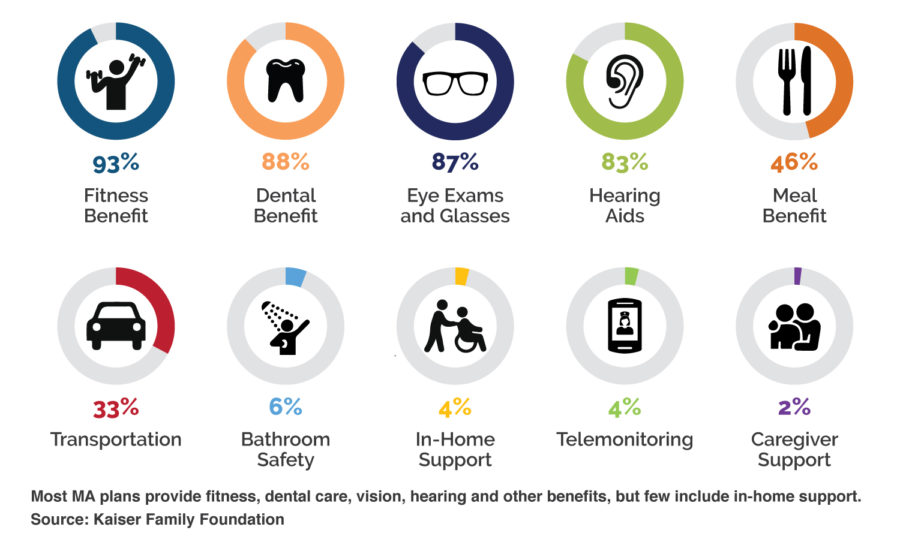
The payer industry is acknowledging what home care providers have long known: It is possible to reduce costs and improve the quality of care by offering wraparound non-medical benefits such as transportation, nutrition services and in-home support.
 Proving value
Proving value
CMS rule changes indicate that the agency sees the value of bringing home care into the MA fold. MA plans are using new benefits to market their services to drive enrollment. But work still needs to be done to use data to prove that supplemental benefits lead to better outcomes—and that the total cost of care stays flat or drops.
The key to scaling these programs will be the ability to unlock data that indicates that providers can proactively keep people safe and well-cared for in their homes and communities and take care of people away from emergency rooms and hospital visits. –Ashish V. Shah, CEO, Dina
Here are six ways for home care providers to get in the MA game:
1. Build relationships
Be bold in your outreach to MA plans. These are early days, so don’t assume that your competitors have outreach figured out. I don’t think health plans understand the home care industry well, but I believe they’re open to working with both large and small organizations that are willing to be partners and share data.
2. Compete with data
Everyone has a story to tell, but you need data to bring your story to life. Start tracking your client base along the lines of living arrangements, safety, how well they understand a care plan and their independence related to daily activities.
3. Emphasize your values
Some bad actors have cast dark clouds over home care, so there’s an opportunity to differentiate yourself with your values.
4. Ask for feedback
After you share your story, ask for feedback. Use this information as an opportunity to learn more about what insurers are doing and how they may be thinking about the market.
This is a growing market opportunity and you want to be there when it scales up.
5. Become a trusted resource
When you have a better understanding of your patients and the direction of the market, you can become a trusted resource and you can drive satisfaction, provide proactive services, and help patients avoid unnecessary hospital and ER visits.
6. Don’t opt out
Don’t say no to patient referrals because they may not have the same financial lifetime value as other types of cases. You want to be in the game, even if those patients aren’t producing a ton of hard value for your organization right out of the gate.
See the full story in HomeCare magazine.

MA Plans are Booming:
How Will You Stay Competitive?
Download our report “Home Benefits Surge in Popularity Among Medicare Advantage Plans” to learn more about leveraging supplemental benefits to increase member satisfaction, retention and STARs.





