
Chronic care management (CCM)is an urgent need as chronic disease is a significant driver of healthcare costs.
Those living with chronic conditions interact with the healthcare system in unique ways and as the number of chronic conditions increases, so do the challenges to managing healthcare. The statistics underscore the size scope of the issue.
The Centers for Disease Control and Prevention (CDC) reports that 90% of the nation’s $3.8 trillion per year healthcare costs can be attributed to people with chronic diseases and mental health conditions.
About 141 million people in the United States were living with one or more chronic conditions in 2010, and this number is projected to increase to 171 million by 2030.
 Nearly 60% of adult Americans have at least one chronic disease. Chronic conditions like diabetes, cancer, and cardiovascular disease are the leading causes of death in this country. More than two-thirds of all deaths are caused by one or more of five chronic diseases: heart disease, cancer, stroke, chronic obstructive pulmonary disease, and diabetes.
Nearly 60% of adult Americans have at least one chronic disease. Chronic conditions like diabetes, cancer, and cardiovascular disease are the leading causes of death in this country. More than two-thirds of all deaths are caused by one or more of five chronic diseases: heart disease, cancer, stroke, chronic obstructive pulmonary disease, and diabetes.
What is a Chronic Condition?
Examples of chronic conditions include, but aren’t limited to: Alzheimer’s disease and related dementia, arthritis (osteoarthritis and rheumatoid), asthma, atrial fibrillation, Autism spectrum disorders, cancer, cardiovascular disease, Chronic Obstructive Pulmonary Disease (COPD), depression, diabetes, hypertension, and infectious diseases like HIV and AIDS.
What is Chronic Care Management?
CCM is designed to support individuals who have long-term health issues that require ongoing medical attention and management, such as diabetes, hypertension, heart disease, chronic obstructive pulmonary disease (COPD), and more. These conditions often cannot be cured completely but can be controlled and managed to improve the individual’s quality of life.
Who is Eligible?
Eligible CCM patients will have two or more chronic conditions expected to last at least 12 months or until the patient’s death and/or that place them at significant risk of death or functional decline. CMS recognizes that chronic care management services are critical components of primary care that promote better health and reduce overall health care costs.
How Does Chronic Care Management Work?
The goal of chronic care management is to improve the individual’s health outcomes, reduce hospitalizations, and enhance overall quality of life by providing people with the necessary tools, resources, and support to effectively manage their chronic conditions. It’s an approach that emphasizes proactive care, education, and ongoing communication between healthcare providers and patients.
Here’s how chronic care management services work:
- Care Coordination: Nurses or care coordinator serve as a point of contact and help coordinate various aspects of the individual’s healthcare, including appointments, medications, and referrals to specialists.
- Regular Check-ins: Care coordinators conduct periodic check-ins, which may occur over the phone or through telehealth services.
- Personalized Care Plans: These plans outline the recommended treatments, medications, lifestyle modifications, and self-care strategies that the individual should follow to manage their condition effectively.
- Medication Management: Ensuring proper medication adherence is crucial for managing chronic conditions. Care coordinators help people understand their medications, dosages, potential side effects, and the importance of taking them as prescribed.
- Education and Support: People are offered education and resources to help them better understand their condition and how to manage it. This may include information about dietary changes, exercise routines, stress management, and other lifestyle adjustments.
- Monitoring and Reporting: Some health plans offer remote monitoring devices that allow individuals to track certain health metrics, such as blood pressure, blood glucose levels, or weight. These devices can transmit data to the care coordinator, who can then identify any concerning trends and take appropriate actions.
Who Can Provide CCM Services?
Only one physician or other qualified health care professional who assumes the care management role for a beneficiary can bill for providing CCM services to that patient in a given calendar month. While services may be provided by a clinical staff person, the service must be billed under one of the following: physician, clinical nurse specialist (CNS), nurse practitioner (NP), physician assistant (PA), or certified nurse midwife. Non-physicians must be authorized and qualified to provide CCM in the state in which the services are furnished.
Improving Chronic Care Management
Many health plans have introduced new approaches to improving care for their members with chronic conditions, including wellness/lifestyle management programs for healthy members, disease management for members with common chronic conditions, and case management for high-risk members regardless of their underlying condition.
Health plans view these programs as a “win-win” and believe that they improve care for their most vulnerable members and reduce cost of coverage.

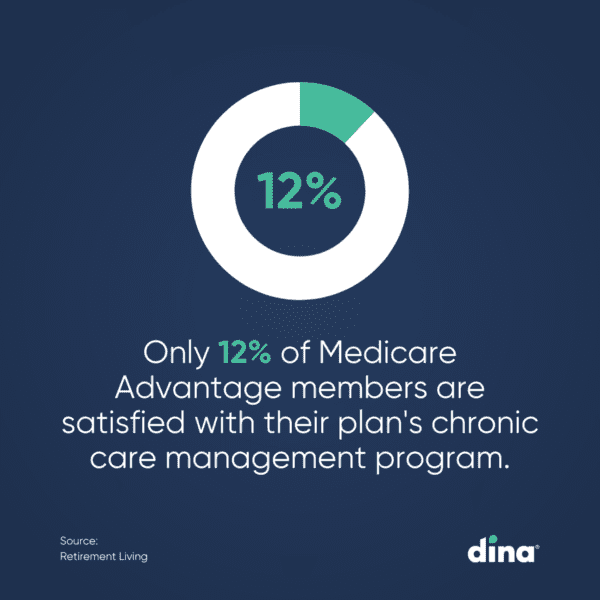
Members might say it’s about time. A recent survey of Medicare Advantage (MA) members reported that only 12% were satisfied with their plan’s chronic care management program. And a report from the Elevance Health Public Policy Institute concluded that MA enrollees find value in plans that meet their personalized care management needs.
Many plans found that chronic care management programs are most successful when they are coordinated with providers and the wider community, including families and community organizations, to raise health awareness and facilitate change.
PACE Members Expect Quick Activation of Home-Based Services.
Does Your Plan Deliver?
See how easy it is to streamline access to medical and non-medical
home-centered benefits, support your centers, and quickly measure results.





