
COVID-19 continues to surge and the Delta variant now accounts for more than 90% of cases in the U.S. In many parts of the country, hospitals are at, or approaching, full capacity.
How can hospitals prepare?
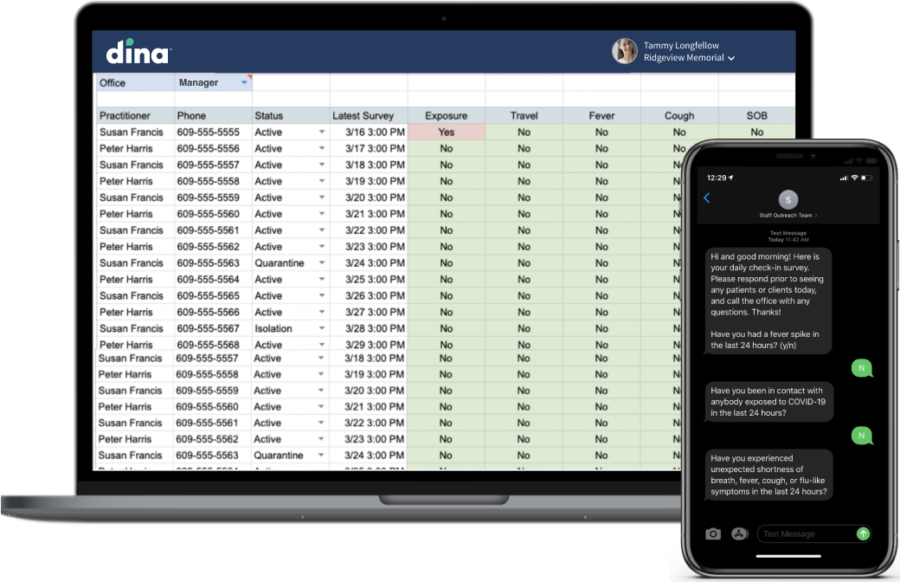
At the height of the pandemic in 2020, our partner Jefferson Health launched Dina’s Covid Care-at-Home remote patient engagement program, using mobile technology to connect with people on a daily basis and track symptoms.
As a result, they were able to quickly extend care to 3,000 Covid-positive patients who were recovering in their homes, and manage escalations in real-time to provide additional support.
Preserving in-patient beds
Jefferson also leveraged the Covid Care-at-Home program to enroll people who presented at the emergency room with symptoms but did not need to be admitted and could be treated at home. This meant inpatient beds across the system could be reserved for those who needed them the most.
Dina recently spoke to Christin Kyriss (below), Jefferson’s director of care coordination, about the team’s experiences during the initial Covid surge, how patients and care teams responded to Dina’s care-at-home technology, and other ways they have deployed remote engagement tools. Here are the key takeaways:
What was the feedback from patients who were remotely connected to their care team at the hospital, especially with the added complications from the pandemic?

This has been a great way to leverage technology and engage with patients in a different way. It’s reduced the phone tag that may result in a delay of care and often causes aggravation on both ends.
How did your nursing team respond to the implementation of new technology?
During the COVID-19 surge, it would have been nearly impossible to provide that level of daily, high-touch outreach with only a handful of nurses to make sure everyone was well-supported through recovery. Our nurses simply would not have been able to provide this level of support on their own.
We were managing escalations by exception so we knew, almost in real-time, exactly who needed our help. When we got that alert, we could reach out by phone to provide further assessment.
Our goal is to establish a cost-effective model that optimizes care and improves the overall patient experience.
Tell us about your new applications for remotely engaging people with chronic conditions.
We’ve identified opportunities to extend care to more patients outside of the hospital, including patients with complex conditions such as Congestive Heart Failure (CHF) and Chronic Obstructive Pulmonary Disease (COPD).
We will soon track device-level data from blood pressure cuffs, weight scales, and pulse oximeters so we get a fuller picture of what’s happening in the home. This model will help us connect with our patients before a minor concern turns into a major health event.
We can help you prepare for Covid surges with low-cost remote patient engagement tools that can be deployed in less than a week, require little training, and don’t need apps or heavy technology support. Reach out to info@dincare.com for more information or a quick demo. Not ready yet? Take a look at this webinar: “The Rise of Home-Based Care: How Jefferson Health is Engaging Patients at Scale.”




