
As of April, Medicaid was serving almost one in four Americans. However, most Medicaid plans struggle to unlock benefits and coordinate personal services that could help seniors stay in their homes safely and longer. This was a central theme of the recent Home and Community-Based Services (HCBS) Conference that was held in Baltimore.
Dina CEO Ashish V. Shah attended the HCBS Conference and spoke to Medicaid executives from across the country. Here are his key takeaways.
Widespread workforce shortages are the biggest challenges facing state Medicaid home and community-based programs. Everyone is constrained with staffing and labor, not only at the planning side of it, but also for those who are helping to fulfill these benefits for in-home services, food, transport, and other services. Building caregiving capacity, and optimizing logistics like who has availability so that members can access benefits in a timely manner is a growing challenge that isn’t going away any time soon.
HCBS Conference Highlights Key Priorities for Medicaid Leaders
Medicaid directors are focusing much of their time around several priorities:
1. Unwinding– As federal policies acknowledge an end to the formally declared public health emergency, state programs will be at the forefront of shaping healthcare changes for millions of Americans. There is evidence that many Medicaid members still don’t understand that unwinding is occurring, don’t know what action to take when they do become aware, 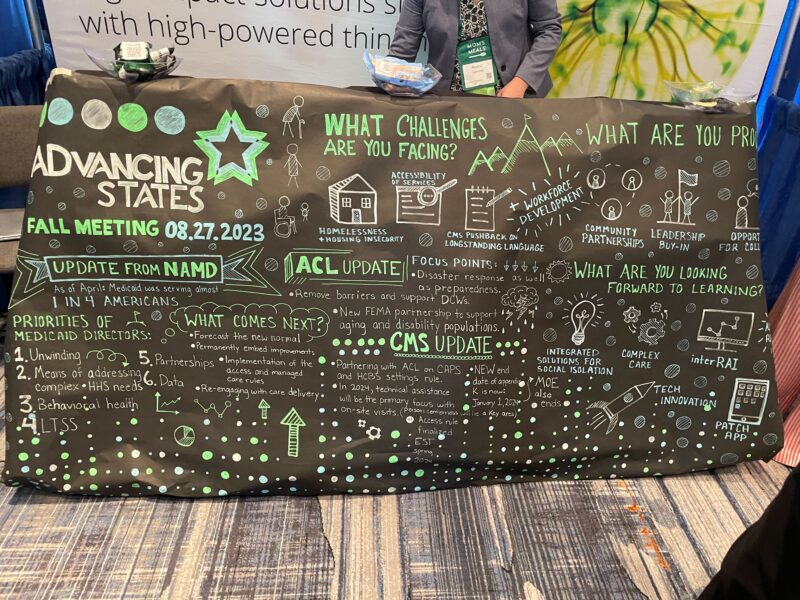
2. Addressing complex care needs– A growing number of people are living with complex care needs and require integrated health and non-medical care to address social determinants of health that address health inequities. Health plans are looking for innovative ways to support complex members and their families in the home and community. Many are starting to prioritize the home as a primary site of care and invest in the tools, services, and partners to support their members aging in place.
3. Data– There is a growing need to make available a suite of both medical and non-medical benefits–and promote utilization–as there is evidence that it will reduce total costs and improve quality/experience. In time, we’ll be able to extract hard data that proves this, and this will lead to a more permanent benefit structure that includes food, housing, personal care, etc.
Proposed Access Rule and its Impact on Quality
Proposed requirements in the Ensuring Access to Medicaid Services rule are intended to increase transparency and accountability, standardize data and monitoring, and create opportunities for states to promote active beneficiary engagement in their Medicaid programs. There is a big emphasis on the timeliness of home and community-based service delivery, in addition to pay transparency and compliance with rules that ensure a majority of the funds are spent on direct care.
There are concerns about the 80/20 payment split. Specifically, the proposed rule would require that at least 80% of Medicaid payments for personal care, homemaker, and home health aide services be spent on compensation for direct care workers. That’s opposed to expenses such as administrative overhead or profit.
One of the many motivators for passing the rule is the potential to delay progression to long-term care facilities and reduce total spend. There is encouraging data that show that a Medicaid member stays in their home 21 months longer versus moving into a nursing home when the appropriate home-based services and interventions are activated.
If adopted, the rules would establish access standards through Medicaid or CHIP-managed care plans, as well as transparency for Medicaid payment rates to providers, including hourly rates and compensation for certain home care and other direct care workers. While this is a positive step forward, there are concerns that it will take years for the rule to be final and implemented, which does not address the current workforce shortages.




