
Since the ACA was implemented in 2009, many healthcare systems have been driving towards lowering costs and improving quality of care. “CMS has committed to moving a certain percentage of our care to value-based care,” said Dr. Kate Behan, Senior Vice President and Chief Population Health Officer at Jefferson Health. “Our payers in many markets are also doing the same. It’s become more important for health systems and provider groups to develop competencies with care delivery models that can deliver on lower costs and higher quality of care.”
Behan spoke at a webinar sponsored by Dina and hosted by Becker’s Hospital Review, where she discussed the expansion of home-based care, new service offerings needed to transition care to the home, and keys to building a successful Hospital-at-Home program.
It’s important for health systems to develop competencies with care delivery models that deliver on lower costs and higher quality of care.
Incentive for Change
“Our two largest value-based care arrangements with payers have over 100,000 patients in them and both have downside risk, so we have some financial responsibility,” Behan said. “Certainly we can do things that are bread and butter for most health systems: try to reduce readmissions and decrease avoidable admissions. But I think to bend the curve in terms of quality and cost you have to start to change your care delivery system in a much more significant way. That’s really where healthcare in the home and hospital in the home comes in.”
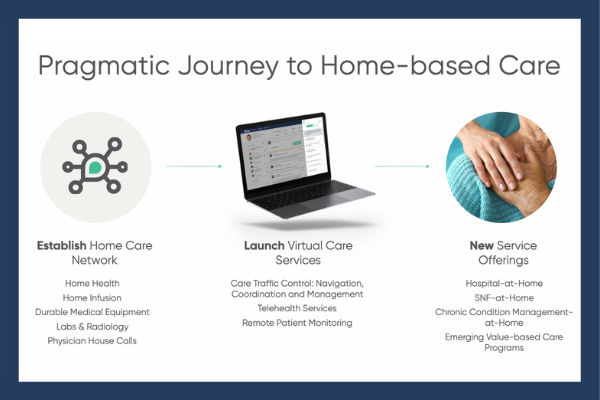
Journey to Home-Based Care
Many organizations have been on a pragmatic journey to establishing a post-acute or home care delivery network with a lot of different capabilities. Some organizations invested early in virtual care services and the market is clearly coming along. Now, we’re moving to the next phases where there is a creative bundling of existing resources and investments in new service offerings.
I think to bend the curve in terms of quality and cost you have to start to change your care delivery system in a significant way.
“When you think about your traditional post-acute care network, we’re focused on looking at the entire continuum: home care, hospice, in-patient rehab, our skilled nursing facility, and outpatient therapy clinics,” said Kristen Vogl, Jefferson Health’s Enterprise Vice President of Post-Acute Care and Musculoskeletal Services.
Broadening Home-Care Services
“Now, we’re changing our focus and asking: What is healthcare going to look like in the future and how will that impact post-acute strategy? Patients are most comfortable in their own homes so we need to think about broadening our home-bound services, our home-care services, and building our primary care visits in the home,” she said.
“We have a lot of these already in the system, so how can we work to further integrate this and provide more care in the patient’s home, which is where they want it. We have to think about things like courier services. How do we get things to patients faster and how do we anticipate what those needs are going to be ahead of the game?”
Read more here about how leading health systems like Jefferson Health prepare for a shift to home-based care. And, you can watch the webinar here.




