Progressive nursing facilities are evolving to operate more similarly to hospitals due to growing engagement in bundled payment arrangements and a devotion to improved patient outcomes. This shift in outcome ownership and shared financial responsibility has led to a need for more efficient patient transitions and increased visibility after the point of discharge. With a national presence, a predominate SNF partnered with Prepared Health to drive real-time communication with their internal service lines and downstream partners to focus on these goals. Within one year, the project’s primary skilled nursing facility saw rehospitalizations reduced by half.
Improving visibility to manage readmission risk
The large portfolio of skilled nursing facilities made it a priority to focus in on specific centers already involved in bundled payment arrangements – some of which were facing readmission rates over 60%. They initiated a project to manage readmission risk with improved visibility across service lines and downstream partners, while also optimizing service line utilization via evidence-based transitions.
Optimize utilization across service lines and reduce leakage
Establishing a supportive partnership from project inception, the team worked closely with the SNF on an extensive analysis of service lines, workflows, and the interactions thereof. Focusing on five BPCI centers, the partnership focused on patient transitions across service lines – reducing leakage and optimizing utilization – as well as to partners for efficiency and visibility through discharge to downstream start of care.
Lowered readmissions and increased acceptance
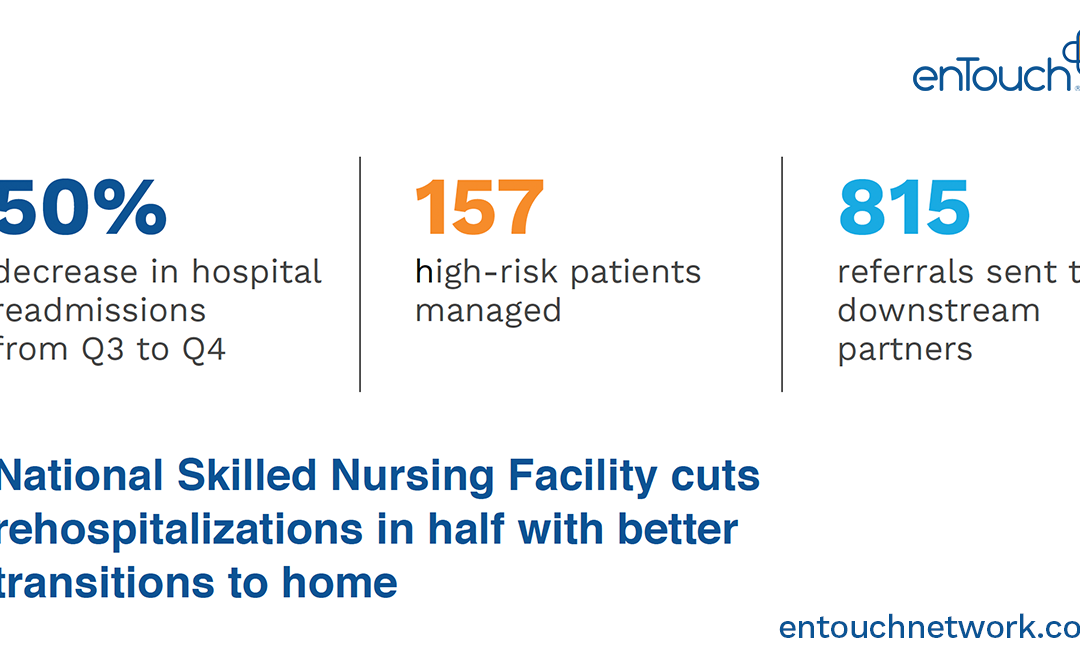
With streamlined transitions and visibility into actual initiation of care which had previously not been available, one facility saw a drastic decrease in readmissions after the implementation of the platform. Even without integrations and an entire conversion to the platform, they saw a 50% decrease in readmissions from Q3 to Q4 in 2017.
The program has seen over 1300 transitions to-date with risk management enacted for 157 high-touch patients with a historically high likelihood of readmission. Focusing the spotlight on the high-volume facility, the social workers sent over 800 transitions through Dina to downstream partners with a referral acceptance rate of 93%.
The facilities also gained visibility and reporting of real-time referral progression through to the actual admission. Allowing teams to see referral admission rates, as well as percentage of accepted referrals that converted to actual admission. This new insight into patient care delivery after the point of discharge allowed social workers to more closely track and ensure care for their highest risk patients.




