
Dina CEO Ashish V. Shah (below) was profiled in HISTalk, where he talked about the impact of the pandemic on at-home care, new payment models for in-home services, and why your home will one day operate like a virtual primary care clinic. Here’s what he had to say:
What effect has the pandemic had on the demand for at-home care as well as the company’s business?
COVID gave us a glimpse of what it’s like when the traditional healthcare system is overrun. Virtual care, whether it’s telehealth or some combination of remote patient monitoring, became critical. But these things need to be complemented by a third, impor
What does the typical care network look like for a senior who has one or more chronic conditions and how do the members that participate in that care network coordinate or communicate with each other?
It’s very complicated. A typical senior or somebody whose health is complex could be on seven plus medications. They may need support with activities of daily living. That’s a non-medical home care service, which is different than a certified Medicare home health type service that may provide skilled nursing and physical therapy, really an extension of a service that you would get in a facility, but now being delivered in a home. So complex med management, personal care support with activities of daily living, perhaps some skilled needs that are required. That’s not even including primary care and specialty interactions.
Virtual care, whether it’s telehealth or some combination of remote patient monitoring, became critical during the pandemic. But these things need to be complemented by a third delivery vehicle, which is in-home care.
A lot of what we do is coordinate all of those logistics so that you can match or exceed the experience that you would receive in a facility. The market definitely wants it, but it’s easier said than done.
How does that care team structure or those care decisions differ for someone who is covered by a Medicare Advantage or a Medicaid Managed Care plan instead of traditional Medicare or Medicaid?
When I work with many folks on the home care side of things, they’re so passionate and they are wonderful organizations. But one of their biggest challenges and obstacles that they face is, how do we ultimately get that care financed that they know that the market needs and that creates value? I love what Medicare Advantage plans and Managed Medicaid plans are doing right now.
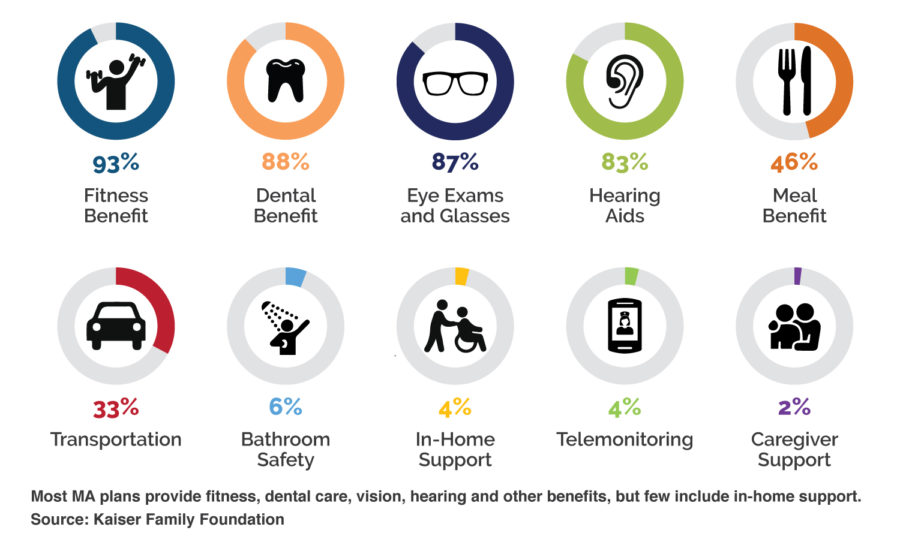
We are in the early phase of supplemental benefits, but this brings online non-medical services or social determinant-oriented services that are paid for, attracting members, but also changing the outcome story.
Medicare, and CMS in particular, were wise to hatch the program years ago and then continue to invest in it and then allow the free markets to innovate. They have a program called VBID, value-based insurance design, that is a vehicle for registering and testing for new types of benefits. If they work, then they ultimately graduate into the scope of things that MA plans can reimburse for. So it’s a really neat program.
On the Managed Medicaid side, in-home services, for example, are covered under what’s called LTSS, long-term support services. This is the goal of trying to meet the member in their home and community and unlocking alternatives to traditional long-term nursing home care. It’s a neat program that has been around for a while, but there’s some complexity in trying to manage that.

For us, it’s really about execution. To simplify our story, we use terms like “care traffic control” to create a visual of equipping hospitals and health plans with the infrastructure to be able to move from monitoring patients in ICU units and in hospital beds and shift that paradigm to coordinating, navigating, activating, and monitoring patients in their homes and communities. The solution we put into the market is a network of resources that are medical and non-medical in nature. We’ve got lightweight technology that allows us to engage with patients and families and understand what’s happening when a healthcare person is not in front of them. We do a lot with data. We bring all that information back to create opportunities to proactively delight that person and meet their needs on a continuous basis.
The organizations that are attracted to that today are health plans, like MA plans or Managed Medicaid, but also large provider groups that have started to go down their path to value-based care. I think that in five to 10 years, this will be everywhere. I don’t think it’s farfetched to think that every home is going to operate like a virtual primary care clinic, where it’s not just your residence, but an actual site of care that the healthcare ecosystem knows how to interact and work with. Our challenge is to make it happen now.
Go to HIStalk to read the full interview.
Want more news about building care-at-home models and staying connected to the home? Sign up for our newsletter for regular industry and company updates.




