
Establishing care-at-home delivery models is a strategic focus for many health systems and health plans. What does it take to replicate the facility-based experience in the home? And is it a viable long-term solution?
“With the variety of payment models that now exist, it’s absolutely possible to establish a financially sustainable care-at-home program,” said Tina Burbine, vice president of care innovation at Healthlink Advisors. “Payers understand that this type of care drives down costs and that’s why they’re entering the market themselves. This means that competition between payers and health systems exists now, and will accelerate over the next few years.”
Burbine was part of the recent Matter-sponsored webinar “The Shift to Hospital-at-Home.” Dina CEO Ashish V. Shah led the webinar and was joined by Dina Chief Medical Officer Dr. Maryann Lauletta, and Healthlink Advisors Clinical Transformation Executive Cynthia Davis. Following is an edited version of the discussion.
Establishing Care-at-Home Delivery
 Shah: Why does hospital-at-home and many of the innovative care-at-home models we are hearing about matter today
Shah: Why does hospital-at-home and many of the innovative care-at-home models we are hearing about matter today
Burbine: Our healthcare market has changed drastically in the past year and it’s enabled many at-home services to be viable care pathways. We have the CMS announcement of reimbursement with the Acute Hospital Care-at-Home Waiver. There are 82 health systems across 33 states that are currently approved for the waiver, and many more are considering entering that process.
Then there’s the influence of payers, who have quickly realized the benefits of this type of care and are willing to participate in reimbursement models.
And in today’s consumer-driven healthcare market, people prefer to receive care in their homes and many are beginning to request it. They’re looking for that from their neighborhood health system and if they aren’t able to provide it, they’ll turn to member plans that may provide it as well. All of these factors converge to create an opportunity for health systems and payers to establish long-term, sustainable programs.
With the variety of payment models that now exist, it’s absolutely possible to establish a financially sustainable care-at-home program.
Shah: What are some criteria to determine who is a fit for care-at-home?
Lauletta: You have to look at the geographic distribution of your patients. Not every patient is able to receive high-level care deliveries in the home. You need to understand: what is the home environment like? Are there any safety concerns or issues with the physical space that you need to address before sending a provider into the home? Is there an internet connection or do you need to provide cellular data cards? And what is the home support system like? Are there caregivers available to assist? And, are there other challenges such as medication management?
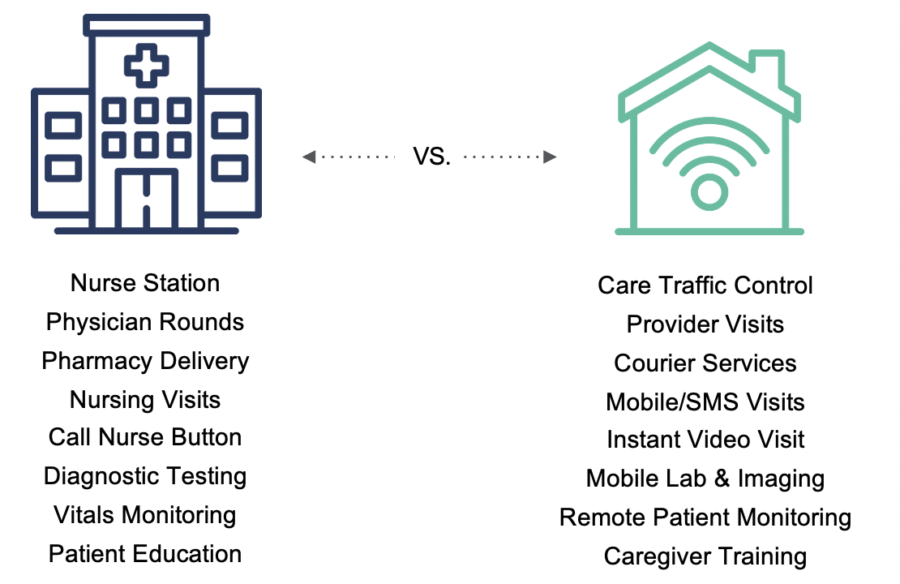
Shah: What is the framework we should start to think through to deliver this type of care in a more standardized model?
Davis: This really is about providing the right care in the right location. You need to look at your strategy to decide how you want to deliver this very innovative care. It starts by ensuring that you have a core leadership team that is creating a vision, looking at 
Then you begin to take a look at: how are you going to provide this care? What’s going to be your staffing model? What sort of clinical protocols are you going to have in place? Some of the heaviest lifting is considering all of your detailed workflows: how are you going to deploy IV medications? Are you going to use nurses or paramedics? Now, you need 24/7 monitoring. What’s your physician and your medical control process?
Finally, you need to examine your payer relationships. Do you have a strong managed care environment in which you might partner with a third-party payer? Many of those payers are beginning to get into this marketplace. Do you want to retain that revenue or do you want to share it with that payer?
You need visibility into what’s happening with your patients when they’re being cared for by providers outside of your scope.
Lauletta: You should also consider your enterprise care team structure. Are you in siloes or do you communicate effectively? Know your processes, policies, and technology. We don’t always talk about it, but there are many gaps and you need a lot of players involved here. They’re usually on different platforms and those platforms don’t always communicate well, but you still need that shared information. You need to be honest and think about what you can do on your own and where you may need to bring in additional resources or technology.
Shah: Oftentimes organizations ask: can we do this by ourselves or do we need to partner with somebody else? What’s the go-to-market approach for introducing this level of service?
Shah: What types of investments do you think make sense?
Lauletta: The most important thing is to have visibility into what is happening with your patients when they’re being cared for by providers outside of your scope, and then having bi-directional communication to intervene or answer questions.

The ideal solution would be a uniform system where your staff is able to communicate in real-time and access patient information while they’re on-the-go. And you need a platform to help you identify high-quality providers who are good stewards of care and good partners, who take your cases in a timely fashion, deliver the services that they say they’re going to deliver and communicate back to you in terms of the outcome.
You need a platform to help you identify high-quality providers who are good stewards of care and good partners.
Shah: Part of Dina’s vision is to build on exactly what you outlined. How do we make it easier to organize key partners, and turn them into trusted delivery partners outside of your four walls? Then, how do we allow them to work together and communicate in real-time in a way that seems like they’re under the same roof? That’s easier said than done, but I think technology plays a key role.
Watch the webinar “The Shift to Hospital-at-Home” to learn more about determining your organization’s care-at-home readiness.




