
Medicaid enrollees who used long-term services and supports (LTSS) had disproportionately high spending in 2020, but just 24% who utilized the benefit did so in an institutionalized setting, according to a recent KFF report.
As the population continues to age, it is likely that more people will need Medicaid LTSS and that ongoing workforce shortages will persist.
States have increased payment rates for long-term services and supports, but it is unclear where additional funding would come from to further increase payment rates and engage additional staff to meet coming demands, according to the report.
Who Uses Long-Term Services and Supports?
KFF found that 5.6 million people used Medicaid LTSS in 2020, but just 1.4 million utilized institutional care. The rest took advantage of home and community-based services (HCBS), a trend that reflects the desire of most senior adults to age in place.
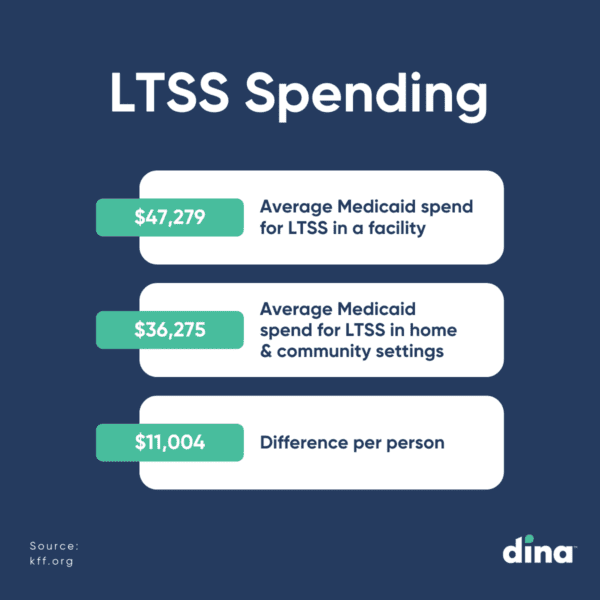
In addition to popular sentiment, LTSS home-based services were found to be less expensive than institutional care. The average Medicaid spend per-person for using LTSS in a facility was $47,279 compared to $36,275 for those in home and community settings, a difference of $11,000.
Staffing Shortages Impact LTSS Delivery
Staffing shortages and high turnover among LTSS workers reflect demanding working conditions and relatively low wages. The Peterson-KFF Health System Tracker found that the number of employees in LTSS settings was measurably lower in June 2023 compared to early 2020.
Workforce shortages have negative effects on the quality of care provided in institutional LTSS settings, and often result in people getting fewer hours or types of HCBS than they need.
This fall, CMS issued a proposed rule to establish comprehensive staffing requirements for nursing homes—including national minimum nurse staffing standards—to ensure access to safe, high-quality care for residents. However, it’s unclear how a mandated increase in LTSS workers will be implemented in the current climate.
Long-Term Services and Supports By the Numbers
In 2020, Medicaid was the primary payer for LTSS, covering over half of all LTSS spending in the U.S. Total spending for the 5.6 million people who used LTSS was nearly $217 billion.
According to the report, Medicaid spending was nearly nine times higher for LTSS beneficiaries ($38,769) compared to regular Medicaid patients ($4,480). Spending was particularly high for those seeking care in facilities.
In addition, those using LTSS comprised 6% of Medicaid enrollment but 37% of federal and state spending, which KFF said reflects the generally high cost of these services.
What are Medicaid Long-Term Services and Supports?
Medicaid LTSS are generally classified by the location in which they are provided: either in an institutional setting or in home- and community-based settings, also known as HCBS.
Institutional care includes care provided in a nursing facility, which is a mandatory Medicaid benefit, and care provided in an intermediate care facility for people with intellectual disabilities, which is an optional benefit that all states currently choose to cover.
HCBS include a broader range of benefits, which are all optional except for home health care. HCBS first became available as a Medicaid “waiver” option and in that capacity, services were generally available to certain types of Medicaid enrollees such as those with intellectual disabilities or those with physical disabilities.
Members Expect Quick Activation of Behavioral Health Services. Does Your Plan Deliver?
In under 2 minutes, we’ll show you how easy it is to coordinate behavioral health and home-centered benefits to your members and quickly measure results.




