The D-SNP market continues to grow to accommodate the rapid rise of the dual-eligible population and ongoing policy changes from CMS that will shape the market.
Beneficiaries who are dually enrolled in both Medicare and Medicaid are cited as a target pocket of growth across a number of Medicare Advantage (MA) plans in year-end results.
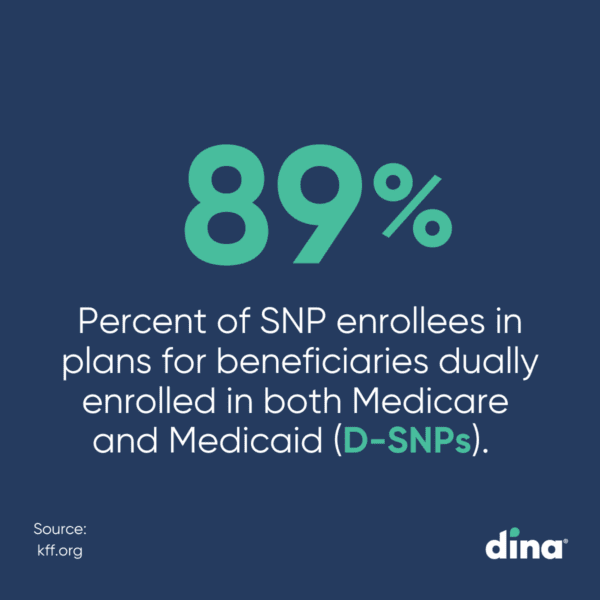
More than 5.7 million Medicare beneficiaries enrolled in MA Special Needs Plans (SNPs) in 2023, double the enrollment in 2018. Nearly 90% of SNP enrollees are in plans for beneficiaries dually enrolled in both Medicare and Medicaid (D-SNPs).
Alongside growth, quality and performance are both in focus as the average Star rating for D-SNPs fell again this year. While notable, this trend is aligned with Star ratings performance across all MA plans.
Considering most plans offer some extra benefits to D-SNP enrollees, it is not clear how often people take advantage of those benefits, if insurers offer adequate networks to access services, and if services are meaningful to a population with diverse health needs.
“In regards to operations, CMS’s signaling around access to benefits and the performance and impact of those benefits seem particularly relevant for SNPs,” said Travis Woyner, Dina’s senior vice president of product.
Now, it’s increasingly on the plans to demonstrate results.
To that end, we spotlight three final or proposed federal regulatory changes, spanning 2020 to 2025, that will drive D-SNPs (and other government-sponsored plans) towards targeted growth, better member communication, and transparency around benefit delivery and usage.
Medicare Advantage and Part D Final Rule
The Medicare Advantage and Part D Final Rule (passed May 2020) includes new contracting limitations for D-SNP look-alikes. Because look-alikes are marketed almost exclusively to duals, they draw dual eligibles away from integrated plan options and place responsibility on the consumer to navigate two separate delivery systems.

Highlights:
- CMS originally identified D-SNP look-alike plans as general enrollment plans whose membership is over 80% dual eligible beneficiaries.
- In the CY 2025 MA Proposed Rule, CMS has proposed lowering this threshold to 70% in 2025 and 60% in 2026.
- California, Massachusetts, and Minnesota have the most plans that would qualify as D-SNP look-alike plans under the proposed thresholds.
CY 2023 Medicare Advantage and Part D Final Rule
Passed April 2022, the CY 2023 Medicare Advantage and Part D Final Rule revises regulations for D-SNPs, and in some cases, other SNPs, related to enrollee advisory committees, health risk assessments, and ways to improve integration of Medicare and Medicaid. “CMS is doubling down on its perspective that a more integrated offering for dually eligible members can add value to the member, to the plan, and to the taxpayer,” Woyner said.
Highlights:
- Enrollee Input on D-SNP Operations: D-SNPs must establish and maintain one or more enrollee advisory committees for each state in which the D-SNP is offered and consult with advisory committees on various issues, including ways to improve health equity for underserved populations.
- New Pathways to Have Star Ratings Specific to the Performance of the Local D-SNP: Star Ratings are calculated at the contract level for MA and Part D plans. In many cases, contracts contain D-SNPs and other non-SNP MA plans, which can make it impossible to fully assess the performance of a specific D-SNP within a specific state.
- New measurement pathways will help identify disparities between D-SNPs and other MA plans and help CMS and states drive quality improvement for dually-eligible beneficiaries.
- Simplified D-SNP Enrollee Materials: Dually eligible beneficiaries have to navigate a complex system of coverage. Currently, most dually eligible beneficiaries receive separate materials (e.g., provider directories) for their Medicare benefits and their Medicaid benefits, which is confusing.
- This makes it easier to understand the full scope of Medicare and Medicaid benefits available through D-SNPs.
CY 2025 Policy Changes: MA, PDP, PACE, & HIT Rule
Given the complex needs of the dual-eligible population, plans continue to offer an integrated, benefit-rich experience for members. In the CY 2025 Policy Changes: MA, PDP, PACE, & HIT Rule changes proposed Nov. 2023 and that entered the House Budget office in Feb. 2024, CMS is making it clear that demonstrating value is critical and more data pertaining to the use of supplemental benefits among D-SNP and other Medicare Advantage enrollees is needed.
In addition, there is concern about marketing benefits such as transportation, dental, and vision, when dual-eligible individuals may already have access to these services through Medicaid.
Highlights:
- CMS has established monthly enrollment periods to favor fully integrated D-SNPs.
- Insurance providers are required to periodically notify D-SNP enrollees if they are not utilizing supplemental benefits offered by their plan.
- Includes greater insight into the experiences of D-SNP enrollees which would be valuable for beneficiaries and policymakers.
Rising Medical Expenses?
Don't Cut Benefits!
Instead, see how to drive smart utilization of non-medical benefits to meet your value-based objectives. Download the report "Rising Medical Expenses? How to Use Supplemental Benefits to Manage Total Cost of Care" to learn more.